Recurrent pericarditis (RP) is a 2 to 3 year journey for many patients,1
THE TREATMENT YOU CHOOSE TODAY COULD MAKE A DIFFERENCE FOR THOSE YEARS
An episodic treatment approach can be a painful experience for patients with recurrent pericarditis.
For U.S Healthcare Professionals Only
of patients with a first episode of pericarditis will develop recurrent pericarditis.2
Approximately
people in the United States seek care for recurrent pericarditis annually.2
There are an estimated
new cases of recurrent pericarditis in the United States each year.2
of patients agreed that they have not fully regained their prior quality of life since experiencing recurrent pericarditis.
of patients were afraid of the potential long-term risks associated with repeated recurrent pericarditis flares.
of patients were willing to take a medication for several years in order to not experience another recurrence/flare.
of patients were diagnosed with other conditions before receiving a recurrent pericarditis diagnosis.
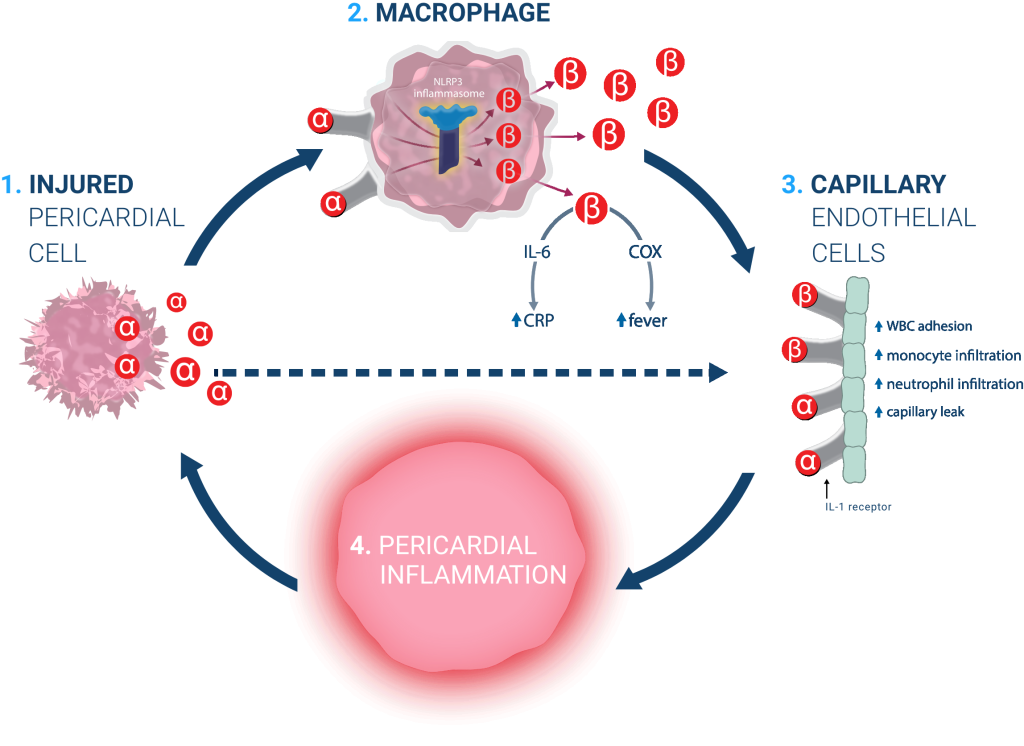
Pericardial cell damage causes release of IL-1α.
IL-1α binds to IL-1 receptors on the surface of macrophages, causing the activation and release of IL-1β in a cascade amplification system.
ENDOTHELIAL CELLS
Active IL-1α and IL-1β bind to IL-1 receptors on the surface of vascular endothelial cells, causing inflammation and additional cell damage.
Additional IL-1-mediated inflammation results in cell damage, causing the cycle of autoinflammation to continue.
Temporarily addressing pain and inflammation associated with a flare.
Preventing future flares by breaking the self-perpetuating cycle of IL-1-mediated autoinflammation that drives the disease.
References: 1. Lin D, Laliberté F, Majeski C, et al. Disease and economic burden associated with recurrent pericarditis in a privately insured United States population. Adv Ther. 2021;38(10):5127-5143. doi:10.1007/s12325-021-01868-7 2. Klein A, Cremer P, Kontzias A, et al. US database study of clinical burden and unmet need in recurrent pericarditis. J Am Heart Assoc. 2021;10:e018950. doi:10.1161/JAHA.120.018950 3. Pericarditis. Cleveland Clinic. Reviewed July 1, 2022. Accessed September 28, 2023. https://my.clevelandclinic.org/health/diseases/17353-pericarditis 4. LeWinter M, Kontzias A, Lin D, et al. Burden of recurrent pericarditis on health-related quality of life. Am J Cardiol. 2021;141:113-119. doi:10.1016/j.amjcard.2020.11.018 5. Data on file. Kiniksa Pharmaceuticals. 6. Kumar A, Sato K, Verma BR, et al. Quantitative assessment of pericardial delayed hyperenhancement helps identify patients with ongoing recurrences of pericarditis. Open Heart. 2018;5:e000944. doi:10.1136/openhrt-2018-000944 7. Adler Y, Charron P, lmazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2015;36(42):2921-2964. doi:10.1097/CRD.0000000000000356 8. Dinarello CA, Simon A, van der Meer JWM. Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat Rev Drug Discov. 2012;11(8):633-652. doi:10.1038/nrd3800 9. Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis. J Am Coll Cardiol. 2020;75(1):76-92. 10. Brucato A, Emmi G, Cantarini L, et al. Management of idiopathic recurrent pericarditis in adults and in children: a role for IL-1 receptor antagonism. Intern Emerg Med. 2018:13:475-489. https://doi.org/10.1007 /s11739-018-1842-x 11. Ridker PM. From C-reactive protein to interleukin-6 to interleukin-1: moving upstream to identify novel targets for atheroprotection. Circ Res. 2016;118(1):145-156. doi:10.1161/CIRCRESAHA.115.306656 12. Vecchié A, Del Buono MG, Mauro AG, et al. Advances in pharmacotherapy for acute and recurrent pericarditis. Expert Opin Pharmacother. 2022;23(6):681-691.
ARCALYST® (rilonacept) is an interleukin-1 blocker indicated for:
Warnings and Precautions
Adverse Reactions
Drug Interactions
For more information about ARCALYST, see full Prescribing Information.